Doctors in these PHCs are concerned about patient load.
Primary Health Center (PHC) authorities said that they face is a shortage of human resources.
Dr. Girija, a PHC Medical officer from Kumbalgudu said, “Here the patient load is more so we are having lack of health staff, though doctors are sufficient, but we have a shortage of staff nurses currently.”
She said that having only one nurse in the PHC means that specific care cannot be given. “There is stress on the staff nurse; she has to take up more work load we have to manage the crowd. We have been here for last eight years and we requisition every year, but not much staff recruitment is done,” she said.
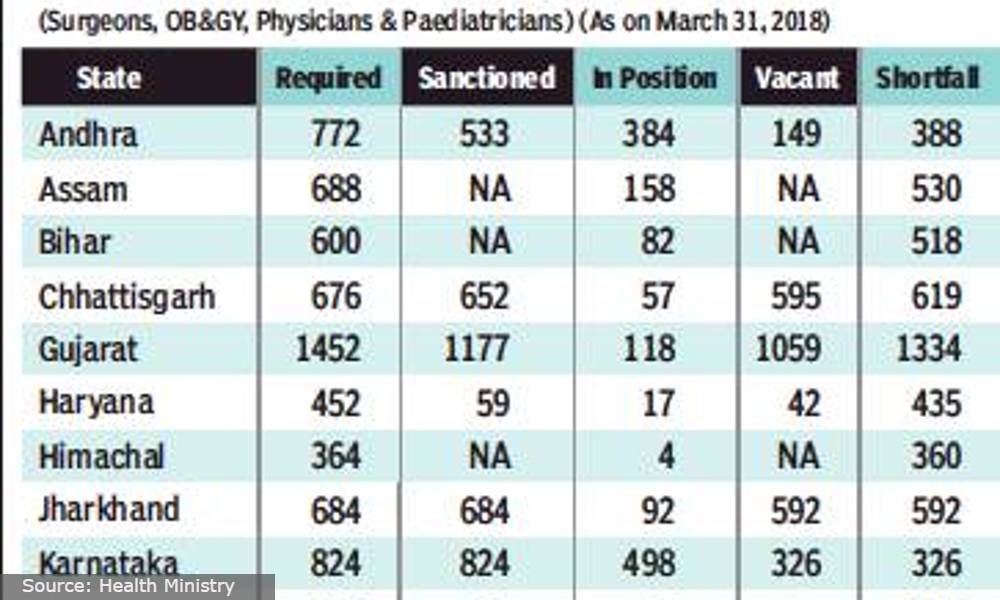
Indian Public Health Standards (IPHS) PHCs states that hospitals require 25,000 doctors across India to tend to a minimum of 40 patients per doctor every day. But with a shortage of 3,027 doctors, 1,974 PHCs are left without doctors and 12 percent of patients go without access to primary health care every day.
Harish Nalawade, Policy Research Associate to the Minister for Health and Family Welfare, Government of Karnataka said that most PHCs do not have the ideal numbers of staff.
Rural Health Statistics Karnataka states that in 2019 – 2020, in 2,380 PHCs and 9,188 sub-centers, there is a short fall of 105 doctors, 606 pharmacists and 327 physicians.
Today’s morbidity and mortality rate may be a result of this shortfall and less community reach with the primary health service said Nalawade, adding that this could be debatable.
According to a report about establishing model PHCs, then Chief Minister Yediyurappa told reporters that the number of doctors would be increased from one to a minimum of three to four.
But Radha, a field worker in a Kumbalgodu PHC said, “We require two doctors for a population of 30,000 – 40,000 people. It is very difficult to handle the patients with just one doctor. If there would be a minimum of three to four doctors it would be much easier to serve our patients.”
Many other PHCs around the area also said they only have one doctor with three nurses and that this poses difficulty for the patients.
Avinash, one of the patients, said he had to sit for long hours before his turn came and until then, he had to bear the pain. “Usually the hospital is crowded with patients, with just one staff it is very much difficult for us as patients to access proper care.”
Hemsesh and Sangeetha also expressed similar grievances of long hours of wait and sometimes patients aren’t given enough care.
Karthik K.L, Project Coordinator of Community Health Center, an NGO said that strengthening PHCs and sub centers will ease the burden of health staff and have a balanced crowd of patients.
“Health work force recruitment in rural areas is not met because of the lack of facilities available for physicians, living condition in rural area is not satisfactory and another major reason is the absenteeism.” said Karthik.
Possible Future Implementation
Nalawade said that making PHC service compulsory for post-graduate MBBS students can help the state deal with the shortage. He added that AYUSH doctors could be recruited if MBBS doctors are not available. He pointed out that Karnataka has selected 25 model PHCs where residential and infrastructural provisions will attract the doctors and paramedical staff.
The Karnataka government is planning to have a medical college in each district adopt a district hospital or PHC in the Public Private Partner model (PPP).





I am so proud of you archana ❤️. Keep doing hardwork !!!