There is no specific HIV sero-surveillance facility for the transgender community in Bangalore; government officials say that there are no immediate plans to establish one.
Currently, there is no HIV sero-surveillance center for transgender people in Bangalore, despite the Karnataka State Policy on Transgender (2017) mandating the establishment of such centers by the government.
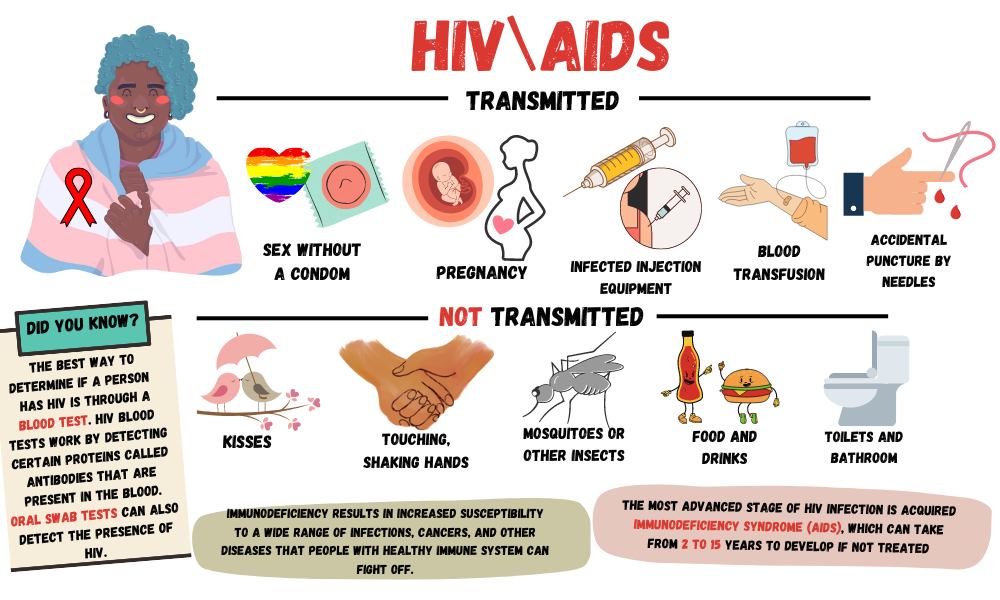
Human immunodeficiency virus (HIV) sero-surveillance involves examining HIV prevalence by testing blood for antibodies against the virus.
Transgender people, living below the poverty line, often face abandonment by their family, forcing them onto the streets where they may turn to begging or resort to sex work for a living, thereby becoming susceptible to diseases like HIV/AIDS. Kajal (name changed), a 37-year-old trans woman living in Sadaramangala, has been diagnosed with HIV. She previously worked as a sex worker and now begs. “When I experience flu or fever symptoms, I visit a nearby clinic and purchase necessary medications from a pharmacy. For more severe issues, I go to Bowring Hospital,” she said. During her last illness, she was admitted to a Tumkur hospital for ten days.
Getting medicines from the hospital is challenging, due to frequent shortage of prescribed medication. Although the policy mandates free medication for trans-persons at HIV surveillance centers, their absence results in inadequate healthcare facilities for this community. For her treatment, Kajal struggles with a lack of support from both her family and community.

Hospitals such as Bowring or Victoria provide antiretroviral therapy (ART) medicines to trans persons. However, as prescribed medicines vary based on tenders with pharmaceutical companies, there is a lack of consistent specialized care, leading to increased side effects among people.
Christy Raj, a trans man working for Payana, a community-based NGO for trans-persons, said, “Many trans persons seeking treatment face challenges in accessing government benefits due to a lack of awareness. Due to the absence of a transgender welfare board, the policy on Transgender is not properly implemented in Bangalore. As a result, there is no government representative to raise awareness about specialized schemes for trans persons. While the Ayushman card offers medical aid up to Rs. 5 lakh for trans-persons, many cannot benefit due to a lack of below poverty line (BPL) cards or other necessary documents.”
He added, “Unlike Tamil Nadu, where state hospitals perform sex reassignment surgeries (SRS), trans persons in Bangalore have to rely on private hospitals, which can be financially burdensome for many. Those taking hormones experience issues like hair-fall, but government hospitals lack treatment options. Additionally, trans women opting for silicone breast implants face side effects without available treatments.”
The Karnataka State Policy on Transgender (2017) was passed based on the landmark NALSA judgment by the Supreme Court in 2014. The objective of the policy was to secure constitutional rights for the transgender community, addressing discrimination in various aspects such as health, education, employment, housing, and protection from harassment and abuse. Despite these intentions, the trans community says that the effective implementation is yet to be achieved.
The officials said that while HIV centers for trans persons are part of the policy, their immediate focus is on the establishment of facilities and programs outlined in the policy. Manasa, probation officer in the Department of Women and Child Development (DWCD) said, “We started the implementation of the transgender policy in 2020, and as of now, we are in the process of establishing the necessary offices. Currently, our primary focus is on acquiring children for the transgender children’s home, and we are reaching out to NGOs for assistance.”
Additionally, no regular employees were specifically hired for the state policy for trans persons. Existing staff, already handling other responsibilities, were tasked with the additional workload, limiting their effort in addressing the policy’s requirements. As a result, the policy for trans community largely remains only on paper.
Bharathi Devi, District Child Protection Officer (DWCD) said, “The Karnataka Women’s Development Corporation is conducting a baseline survey specifically for trans persons in Karnataka. Two districts have been completed, and the survey in Bangalore is yet to take place. Once the survey is concluded, we’ll have detailed information about our target group, allowing us to concentrate on establishing HIV screening centers.”

Stigma surrounding HIV and financial instability often lead trans women to continue engaging in sex work even after learning they are HIV positive, contributing to the spread of the infection to others. Sister Salya, working with Dream India Network, said, “In RPC layout, many trans women are sex workers, but when approached, they often avoid direct discussion, referring to HIV as ‘Lady sickness.’ Despite a large number being HIV positive, stigma prevents many from acknowledging their condition. Those who reach out are directed to Milana NGO for medical assistance, as government hospitals often fail to provide proper guidance to transgender individuals. The trans community, particularly sex workers, faces challenges accessing healthcare due to identity-based stigma.”
In many countries, trans women face marginalization, victimization, and stigma. Experts say that despite effort in recognizing transgender rights in India, there’s still a lack of support and human rights protections for the community. Swathi SB, researcher at the Institute of Public Health, Bangalore, said, “Trans women who are sex workers not only face high rates of sexually transmitted infections (STI) and HIV, violence, stigma, and discrimination, but also have a lower education rate compared to other stigmatized and high-risk populations for HIV. This results in a lack of respect and economic opportunities, ultimately affecting their health and well-being.”
She added, “The government needs to provide them with focused education, and community outreach programs to destigmatize HIV. It is also essential to provide them with accessible healthcare services which aligns with their specific needs is essential. Creating supportive environments for their psychological well-being and effective implementation of the policy are steps to break the cycle of discrimination among this marginalized group.”