The pandemic has led to a rise in the use of antibiotics; making already resistant bacteria that cannot be killed by antibiotics stronger.
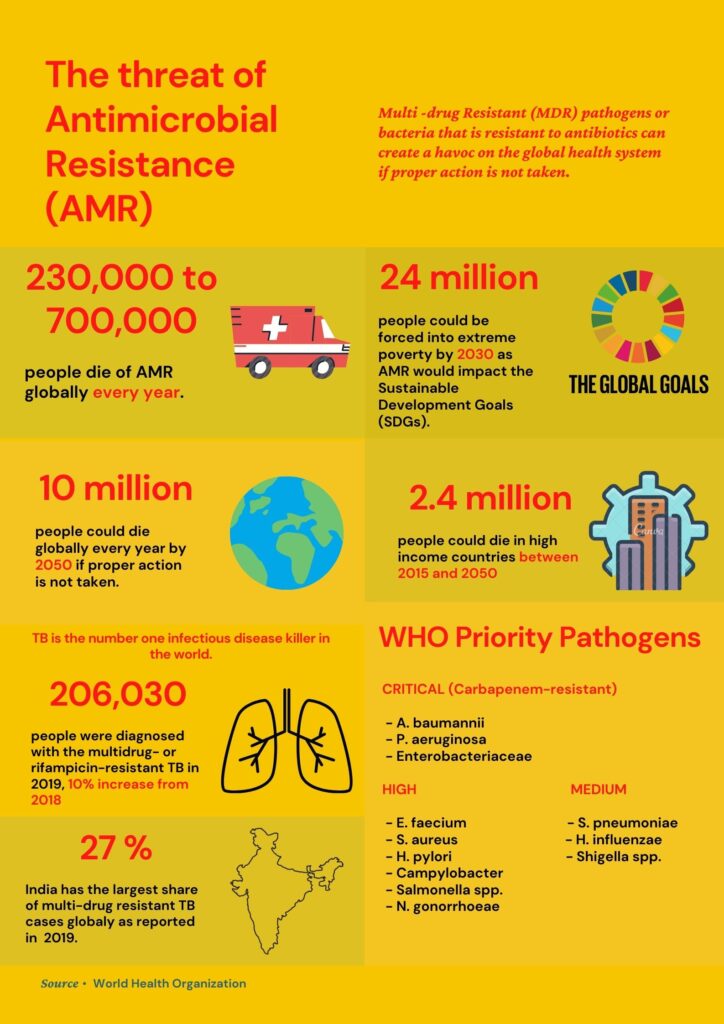
Bengaluru: Researchers now believe that critical Covid-19 patients are likely to be more vulnerable due to antimicrobial resistance (AMR), which is the growing resistance of microbes against antibiotics. In 2019, the World Health Organization (WHO) had warned that if no action is taken on the crisis of AMR then it could lead to 10 million deaths each year by 2050. This estimate was before Covid-19.
“There is no threat. It is already out of hand. A threat is when you are thinking whether it will happen or not. In the case of antibiotic resistance, we are already living in a catastrophe,” said Dr Santanu Datta, the Chief Scientific Officer (CSO) at the BUGWORKS Research Private Limited.
AMR is a term referred to the overall resistance of microbes such as parasites, viruses and fungi. Overuse of antibiotics has led to bacteria getting stronger due to which treating patients with bacterial infections has become harder.
One of the most common reasons of rising antibiotic resistance is lack of awareness in people as well as laxity in following prescriptions. Dr Biplab Jamatia, MD in Community Medicine said, “Many times people are not careful in completing the prescribed dosage. If they have a prescription for five days, they might take the medicine for only two days.” Dr Jamatia explained that this leads to the bacteria getting more resistant so the next time the same medicine or dosage would not work for the same symptoms.
Another factor that leads to antibiotic resistance is people buying antibiotics without prescriptions. Dr Datta said, “Officially, people cannot buy strong antibiotics without prescriptions. But in India many people do not have the money to go to a doctor and get a prescription so they buy from chemist shops without prescription as much as possible.”
Hiding in Plain Sight: Secondary Bacterial Infections
Dr Datta said that the pandemic has exacerbated the situation that was already out of hand. “Whatever antibiotics were used; they will now be used ten times more. Nobody is testing whether the antibiotics would be effective or not. We have done some testing and found out that most of the antibiotics are not working.”
A 2020 research paper published in the American Society for Microbiology stated that secondary bacterial infections occur in many COVID-19 patients and can be associated with worse outcomes. The researchers found that the highest percentage of bacterial infections was detected among critically ill patients. “If you take any Covid-19 prescription, you will see that there is always one antibiotic prescribed,” Dr Datta said. The WHO also reported that a review of studies published on hospitalized COVID-19 patients identified that 72 percent of patients received antibiotics.
One more aspect that remains hidden from people is that hospitals are full of infections. This means that a patient with a minor problem could contract an infection in the hospital that is potentially deadly if the bacterium is drug resistant. These infections are known as Hospital Associated Infections (HAI). Dr Datta said, “Around 30 percent of people who die in hospitals die of hospital acquired infections which are mainly infections not related with the primary cause of visiting the hospital.”
“My father-in-law was admitted for a simple gall bladder operation but somehow he contracted pneumonia two days after getting admitted,” Savita Thakur, working from home in Punjab, said. Hospital Acquired Pneumonia (HAP) is one of the most common forms of HAI. A patient could contract it within 48 hours or more after they get admitted to the hospital.
Thakur was scared because it was in the middle of a pandemic and the doctors thought that pneumonia was an indication of the coronavirus. However, after two negative Covid tests and shifting him to an ICU, the doctors said they had no idea how the lung infection developed. “Imagine going for a minor operation and admitting him in the ICU for 10 to 12 days. It was horrible emotionally and financially.”
Choosing between profit and life
A WHO report on an analysis of the antibacterial clinical development pipeline stated that the efforts of discovering new antibiotics were “insufficient to tackle the challenge of increasing emergence and spread of antimicrobial resistance.”
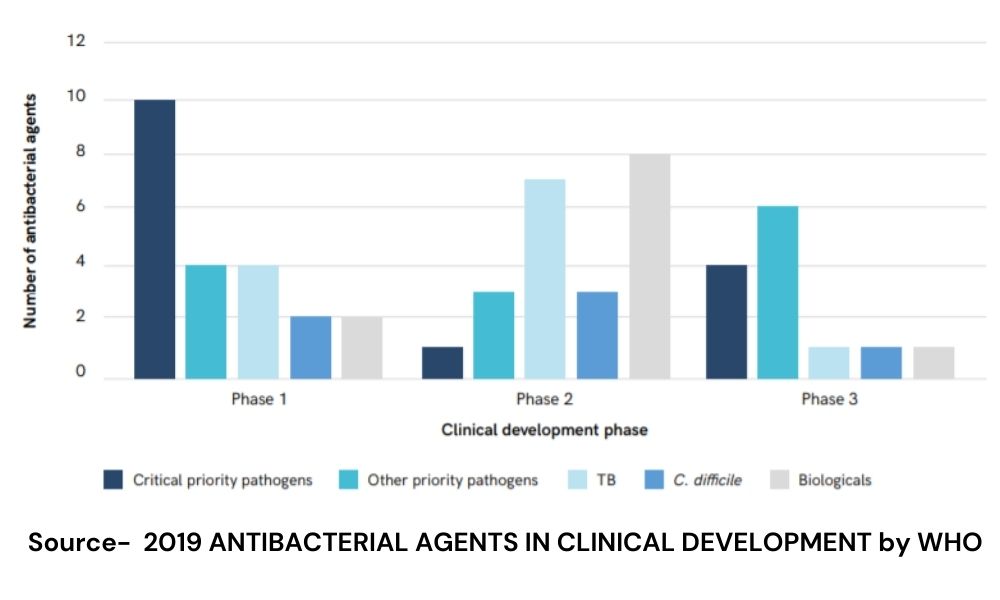
Dr Datta said that big pharmaceutical companies have stopped investing in antibiotics mainly because drug discovery is expensive and a very complex process. He added that since antibiotics are cheap and are prescribed for a short duration, it is not very profitable to invest in making new antibiotics. “Market dynamics are such that unless the government helps you out, it is not very profitable,” he said.
On the macro-level, AMR has become a public health crisis.
In 2017, the Indian government had released the National Action Plan on Antimicrobial Resistance (2017-2021) developed in partnership with the WHO. It was put in place to improve awareness, strengthening knowledge, promoting research, controlling infection and optimizing use of antimicrobial agents in health and food.
Dr Datta said that in a country where there is a huge gap in access between the rich and the poor, executing an AMR policy is not possible. “The system is broken. AMR is not the only problem but it is connected with many other problems,” said Dr Datta. “When there are multiple holes in the system, you cannot fix one hole. AMR is one of the big holes but it cannot be fixed in isolation.”
Doctors said that using antibiotics judiciously and selling antibiotics with proper prescriptions are some of the ways to tackle AMR. Dr Datta said that the only way this can be seriously tackled is if the government provides funds into the Research and Development of new antibiotics. The government also has to make people more aware about the existence of another global health crisis that is still behind the veil.




